In this post, we will discuss about the science of disc protrusion, herniated disc, and treatments including cortisone injection
Different types of disc injuries
There are also different types of disc injuries and sciatica depending on the cause. Disc injuries can be classified into three categories: discogenic disorder, disc protrusion, and disc degeneration. The typical terminologies we use are disc protrusion and herniated disc.
Discogenic Disorder: This occurs when the annulus fibrosus, the outer layer of the disc, is slightly torn, allowing the nucleus pulposus to leak into it. When it comes into contact with nerves, it causes inflammation and leads to lower back pain.
Disc Protrusion: In this case, the annulus fibrosus is more severely torn, causing the nucleus pulposus to protrude outside the disc and compress the spinal nerves. This can result in symptoms such as lower back pain and radiating pain in the legs.
Disc Degeneration: Disc degeneration occurs as a person ages, causing the disc to lose its water, become stiff, and decrease in height. This loss of cushioning ability in the disc can lead to lower back pain.
Why are disc injuries so painful?
There are mainly two scenarios in which a disc can cause pain. One is discogenic low back pain, which occurs when the inside of the disc is damaged, and the other is sciatica, which results from a protruding disc. This is what people mean when they say their legs hurt because of a herniated disc. When the gel-like substance inside the disc leaks and impinges on the nerve leading to the leg, it can cause significant leg pain called sciatica.
Mckenzie Extension

McKenzie exercises are a type of physiotherapy developed by Robin McKenzie in New Zealand. These exercises involve stretching the body to relax muscles, increase flexibility, reduce pressure on the front of the discs, and promote healing of damaged posterior annulus fibrosus.
In the first step, you start in a comfortable prone position. In the second step, you use your elbows to gently arch your lower back. In the third step, you extend your arms to further arch your lower back. Finally, the fourth step involves standing straight and arching your lower back. It’s important not to exert excessive force on your lower back during each movement, and you should progress to the next step only if you can perform each stage without experiencing pain. Additionally, it’s crucial to stop the exercise immediately if you experience any pain.
It is important to do this exercise but we should also note that Mckenzie exercise is not the cure, but maintaining extension of the lumbar spine is the cure. Mckenzie exercise is only a part of the treatment for disc rehabilitation.
Why is Extension good for the disc?

A lumbar disc behaves like a water cushion, shifting its nucleus pulposus back and forth as the lumbar spine moves. When you bend forward (flexion), the nucleus pulposus moves backward, exerting pressure on the posterior annulus fibrosus. Excessive force applied while bending, even repetitive or prolonged flexion, can put pressure on the annulus, leading to the tearing of the annulus fibrosus and the onset of disc-related pain. If the pressure on the nucleus pulposus continues, it can cause the complete tearing of the posterior annulus fibrosus, resulting in disc protrusion.
Conversely, when you arch your lower back (extension), the nucleus pulposus shifts forward, causing a narrowing of the posterior annulus fibrosus. The posterior annulus fibrosus thickens and the torn sections come into contact and adhere to each other. This presents a golden opportunity to mend the torn posterior annulus fibrosus. There is no need to worry about the anterior annulus fibrosus tearing while extending, as it is naturally thicker than the posterior annulus fibrosus.
The extension movement serves to push the nucleus pulposus forward, thicken the posterior annulus fibrosus, and promote the healing of any injuries to the posterior annulus fibrosus. Therefore, it prevents the nucleus pulposus from causing damage to the posterior annulus fibrosus and protruding backward.
Hence, the extension movement not only strengthens healthy discs but also aids in the healing process of damaged discs. The exercise is straightforward, yet it has such a beneficial effect on the discs that there is no reason for individuals with lower back pain, sciatica, or a history of previous lower back issues to refrain from doing it. If you are currently experiencing lower back pain or are concerned about the recurrence of lumbar pain due to a history of back problems, it is advisable to incorporate extension exercises into your daily routine frequently.
Should you have surgery on a herniated disc?
This is a matter of whether a disc regenerates by itself or not. If the protruded part of the disc can reduce by itself and the pain is not too severe, then there wouldn’t be a need for surgery. This is why pain is a big factor for doctors to decide whether to perform surgery or not. But recent studies suggest discs do reduce by themselves.
According to a research, 10~40% of people who had back surgery reported to have failed back surgery syndrome (FBSS). (1)
This means that at least 1 out of 10 patients face acute complications following surgery. Furthermore, as for late complications, it is known that 5 to 20 out of 100 patients experience conditions like post-surgical instability of the spinal segments or severe pain, known as post-surgical failed back syndrome.
In addition, it becomes very difficult to recover with rehabilitation if the patient has already had back surgery.
So if you have disc injury, and the pain is unbearable, you should get a injection or surgery. But even if you have a huge disc protrusion and its not too painful, then you shouldn’t get any surgeries. Also if you have sciatica which is running down both your legs or weakness in the legs, or bowel and bladder symptoms, it is recommended you get surgery as the disc may be pressing firmly on multiple spinal nerves and these are difficult to recover by rehabilitation.
Research on Disc and Sciatcia
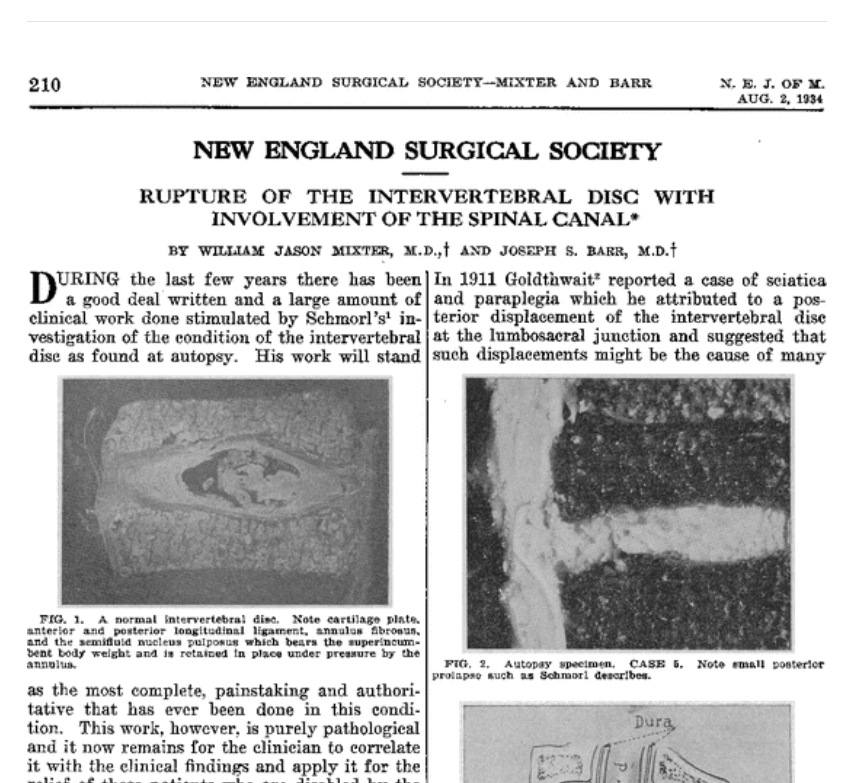
Sciatica was initially thought to be caused by the sciatic nerve itself, but was discovered to be due to the nerve root being compressed by disc in 1934 by William and Joseph. (2) It therefore meant that the protruded disc must be removed in order to reduce sciatica.
Verne T. Inman in 1947 (3) and Michael Kelly in 1956 (4) stated an objection to this as there are cases where sciatica resolves by itself even without surgeries.
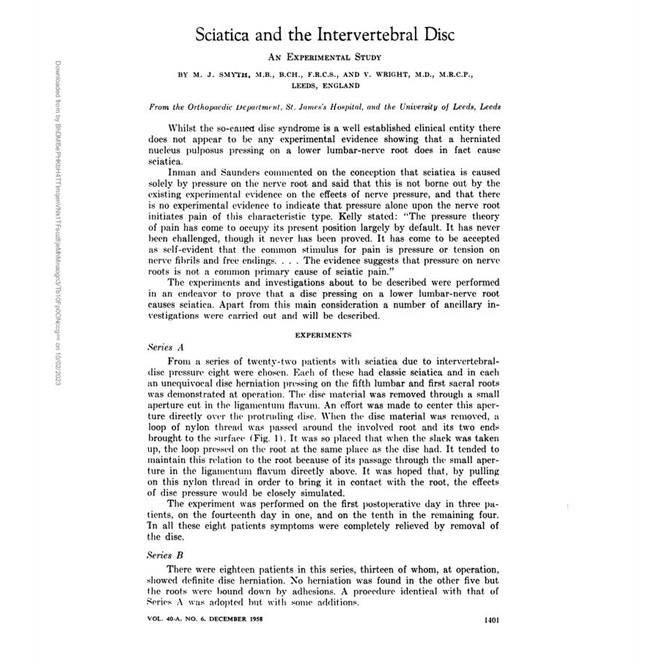
To prove this, Smyth MJ in 1958 left a nylon thread behind the nerve root that had disc pressure and underwent disc surgery, and also behind a normal nerve root. The thread was hanging out of the skin so that when the thread was pulled, it would put pressure on the nerve root and cause sciatica. The nerve root which had previous disc injury caused sciatica when it was pulled by the thread, but the nerve root that did not have disc pressure did not reproduce sciatica. (5) This was a surprise as the normal nerve root did not reproduce sciatica when the nylon thread was pulled, because it was against Smyth’s hypothesis.
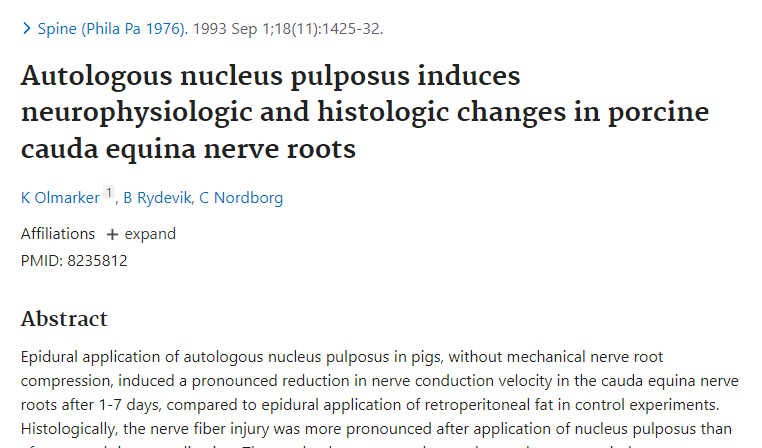
Olmarker K. in 1993 (6) conducted an experiment in which he extracted the nucleus pulposus from pig lumbar discs and injected it on the tail nerve roots. The nerve roots were not mechanically compressed; only the nucleus pulposus was applied to the nerves. Approximately three days after the nucleus pulposus was applied, the conduction velocity of the nerve roots, which was originally 60 meters per second, dropped to 30 meters per second. Additionally, microscopic examination of the nerve roots revealed a severe inflammatory response and observable nerve damage. This discovery revealed that not only does a herniated disc mechanically compress nerve roots causing sciatica, but also the herniated material (nucleus pulposus) can lead to inflammation when it comes into contact with the nerve roots. This breakthrough solved a longstanding mystery in the field of sciatica.
This study was repeated in dogs by Olmarker K. and Otani K. which reproduced the same effect. (7)
Therefore, it was discovered that in cases where a disc mechanically affects the nerves but does not result in sciatica, we learnt that inflammation occurred and then subsided. Furthermore, it was learned that the reason sciatica can occur without a clear demonstration of disc herniation is that even when there is no visible compression, a torn disc can release its nucleus pulposus, which can then come into contact with and inflame the nerve roots.
Olmarker’s experiment solved the mystery of Smyth’s research. In Dr. Smyth MJ’s research, in cases where the nerve roots were compressed by disc herniation and had nucleus pulposus embedded in them, inflammation was present. Therefore, when pressure was applied to these inflamed nerve roots by nylon thread, it resulted in sciatica. Conversely, in the case of normal nerve roots without inflammation, applying pressure did not cause pain. It was a matter of whether the inflammation is present or not in the nerve root, that it causes sciatica when compressed.
In Dr. Otani’s experiment (7), additional finding was observed that the nerve conduction velocity in dogs initially slowed down the most on the seventh day after applying the nucleus on nerve roots. However, after one month, it gradually improved, and by two months, it had completely returned to normal. This discovery indicated that there is a natural course of recovery for nerve roots inflamed due to disc herniation, even without specific treatment. Of course, dogs and humans have different recovery time, so this must also be taken into account that humans don’t recover in 2 months and also depends on the severity of the disc damage and inflammation.
What’s more intriguing is that dogs in the experimental group, who had undergone disc experiment within one to six months, were subjected to lumbar MRI scans. Among them, those who had punctured holes in the discs (from the experiment) exhibited much more severe disc degeneration, and one of them even had herniation. This confirmed the fact that creating holes in the discs accelerated disc degeneration. This is why I personally do not recommend discography because it creates holes in the disc.
Disc herniation is the process in which the nucleus pulposus, which was securely contained within the annulus fibrosus, ruptures through the annulus fibrosus and protrudes outside the disc. Inside the nucleus pulposus, there are living cells. However, when it escapes outside the disc, it becomes deprived of essential nutrients and oxygen, leading to cell death. In the process, inflammatory substances are released from the dying nucleus pulposus cells, which can come into contact with the nerve roots, resulting in inflammation. However, once inflammation occurs, it tends to subside over time, and when all the nucleus pulposus cells have died, no more inflammatory substances are produced. As a result, the inflammation of the nerve roots naturally decreases and eventually disappears. Therefore, discs can heal on their own without the need for surgery.
Cortisone Injection

In 2001, J. Karppinen published the results of a clinical trial. Patients with sciatica caused by disc herniation were randomly divided into two groups. One group received steroid injections, while the other group received an equal amount of saline solution, essentially a placebo with no therapeutic effect. The study observed the changes in sciatica in both groups. The results showed that, after approximately six months, both groups experienced significant relief from sciatica. This study demonstrated that steroid injections had an early pain-reducing effect (within the first six months) but showed no significant difference after one year. (8)
However, having a vague aversion to anti-inflammatories or steroid injections is not a helpful approach to treatment, and blind faith in them is also not advisable. When the pain is extremely severe, receiving injections can be the right course of action.
Steroid injections work by reducing inflammation and alleviating pain for approximately two months. The meaning of these two months is crucial. During this period, if the disc heals, even after the medication wears off, inflammation and compression will no longer occur, preventing the return of pain. However, if during these two months, a person frequently engages in activities that strain the spine, there is a risk of pain recurrence when the medication wears off. In essence, the injections are like extinguishing an urgent fire, while the rest of the healing is part of the natural course of disc recovery.
Reference
- Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
- Mixter, W. and Barr, J. (1934) Rupture of the Intervertebral Disc with Involvement of the Spinal Canal. The New England Journal of Medicine, 211, 210-215.
http://dx.doi.org/10.1056/NEJM193408022110506 - INMAN VT, SAUNDERS JB. Anatomicophysiological aspects of injuries to the intervertebral disc. J Bone Joint Surg Am. 1947 Apr;29(2):461-75. PMID: 20240207.
- KELLY M. Is pain due to pressure on nerves? Spinal tumors and the intervertebral disk. Neurology. 1956 Jan;6(1):32-6. doi: 10.1212/wnl.6.1.32. PMID: 13280025.
- SMYTH MJ, WRIGHT V. Sciatica and the intervertebral disc; an experimental study. J Bone Joint Surg Am. 1958 Dec;40-A(6):1401-18. PMID: 13610969.
- Olmarker K, Rydevik B, Nordborg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots. Spine (Phila Pa 1976). 1993 Sep 1;18(11):1425-32. PMID: 8235812.
- Otani K, Arai I, Mao GP, Konno S, Olmarker K, Kikuchi S. Experimental disc herniation: evaluation of the natural course. Spine (Phila Pa 1976). 1997 Dec 15;22(24):2894-9. doi: 10.1097/00007632-199712150-00012. PMID: 9431625.
- Karppinen J, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, Nieminen P, Ohinmaa A, Tervonen O, Vanharanta H. Periradicular infiltration for sciatica: a randomized controlled trial. Spine (Phila Pa 1976). 2001 May 1;26(9):1059-67. doi: 10.1097/00007632-200105010-00015. PMID: 11337625.

Pingback: Herniated Disc in the Lumbar Spine and Disc Management - Hornsby Chiropractor
Pingback: Cervical Disc Injury - Hornsby Chiropractor